Overview
The average length of stay metrics in Strategy are calculated from all discharge claims submitted by the listed facility during the standard one year reporting period from the time of patient admission to discharge. The metric is calculated in days.
![]() To get the average, we add up the count of days from all eligible stays and divide by the number of stays.
To get the average, we add up the count of days from all eligible stays and divide by the number of stays.
More detail
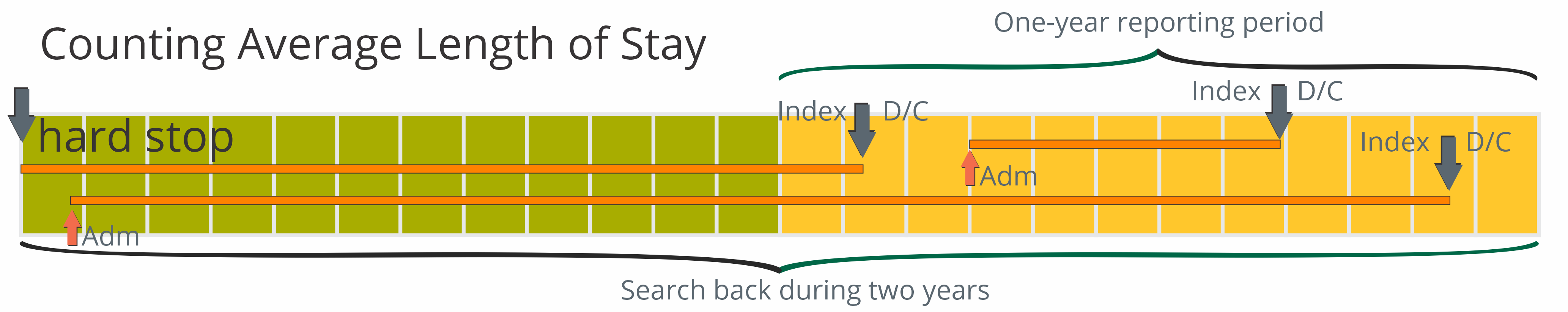
To calculate an average length of stay, we start by looking for a facility discharge. This index event must be on a claim submitted during the most recent one year reporting period, or, in the case of trended metrics, in the quarter for which the count is to be calculated. From that date we look back for an admission or to the start of the reference period. The reference period for counting the number of days in a stay is within two years prior of the end of the most recent quarter of data. See the image for details.
Example:
The image below shows two years broken into the twelve months presented as separate blocks.
The twelve blocks on the right represent our standard one-year reporting period; the period from which we gather our index events. The index events in this example are discharges from care at the organization for which the metric is being calculated.
The twelve blocks on the left show the extended counting period. We count the days from the discharge back to an admission, or to the start of the reference period. As you can see from the image, a stay must begin during this two year reference period.
The skinny rectangles represent patient stays. As long as the discharge (D/C) occurs during the one year reporting period.
![]() Length of stay calculations in all Marketscape Insights modules include only patient stays where the patient has been discharged. As a result, length of stay metrics will not include some patient stays of any length that occur during the two year period. For example: a patient who has been in hospice care for over a year, but not discharged, would not appear in our length of stay metrics even though that would extend the length of stay average.
Length of stay calculations in all Marketscape Insights modules include only patient stays where the patient has been discharged. As a result, length of stay metrics will not include some patient stays of any length that occur during the two year period. For example: a patient who has been in hospice care for over a year, but not discharged, would not appear in our length of stay metrics even though that would extend the length of stay average.
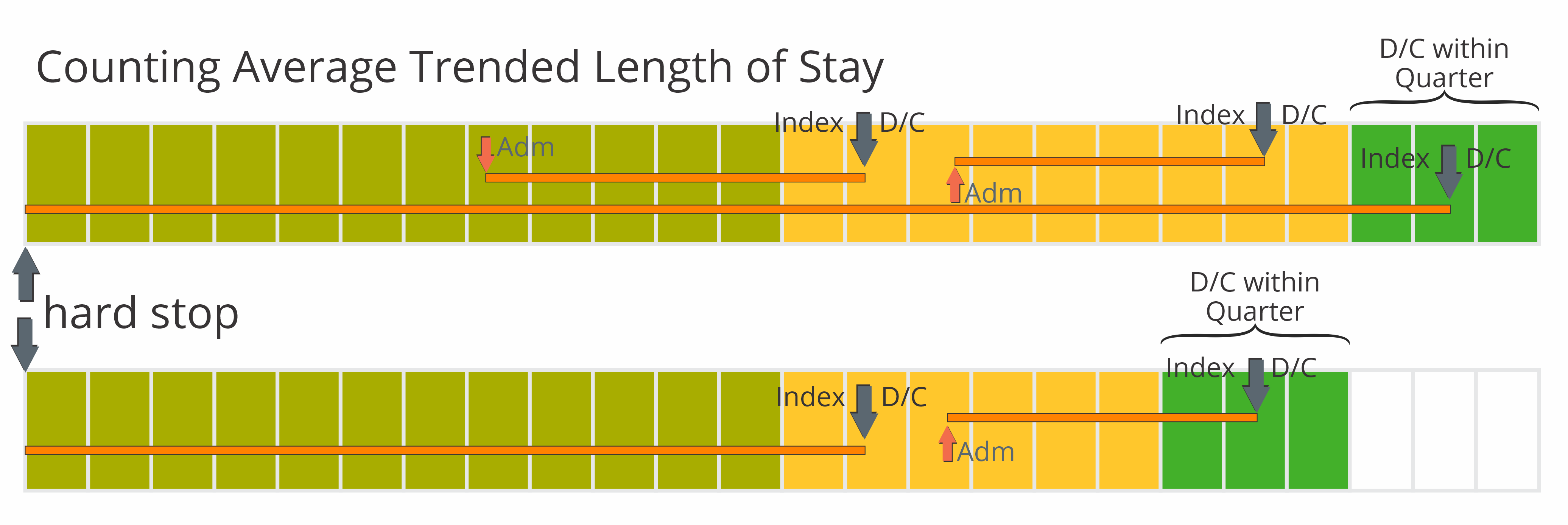
Trended ALOS
In some tables we display trended quarterly length of stay metrics. The length of stay metrics are calculated in the same way, with one exception. The reporting period in which we look for discharges is a quarter rather than from the entire year.
To get the trended quarters, we look at each quarter in our one year reporting period for discharges within the quarter. We then look back through the two year reference period that aligns with the end of the quarter. As you can see from the image below, we only count days during the two year period prior to the end of the most recent quarter of data and do not count any days earlier.