Overview
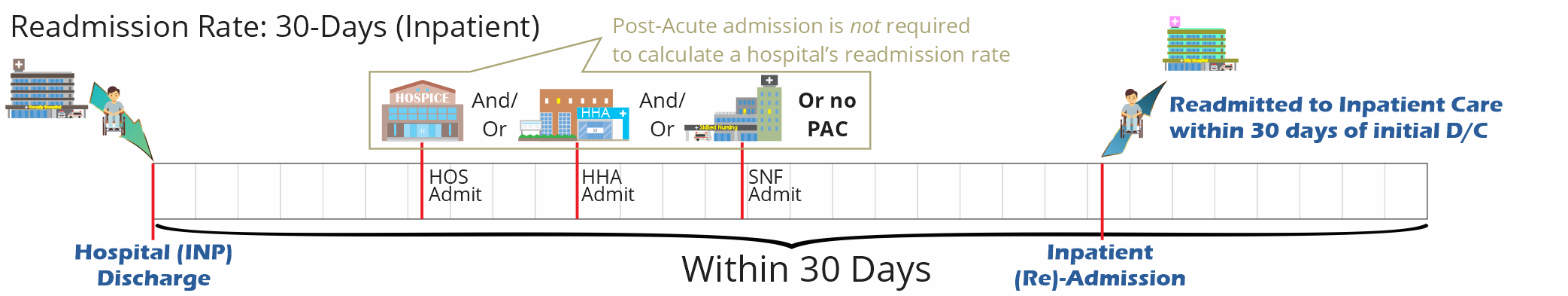
A readmission is a care event where a patient is admitted to any inpatient stay within 30 days of being discharged from an inpatient stay. Like this: INP D/C ![]() INP (RE)Admission within 30 days.
INP (RE)Admission within 30 days.
The Trella Health Readmission Rate is a percentage measurement of readmissions against a select population. This rate can be calculated for either hospitals or post-acute agencies. Please see below for lots of information on calculation.
 In this article
In this article
- Similar Metrics
- Usage
- Calculation
- Reporting Periods
- Trended Readmission Rates
- Inpatient versus post-acute readmission rates
- Deep in the weeds: Exceptions/Inclusions
- Unique SNF metrics
Similar Metrics
Although readmission rates are primarily a performance metric used to evaluate a hospital's success, Trella Health slices the data in numerous ways to present different perspectives on readmissions.
Readmission FFS and MA
Readmission rate metrics are available for both Medicare FFS and Medicare Advantage. Look for "FFS" or "MA" in the header name to identify which is which.
PAC Readmission
Since post-acute care is so significant for patients, and since Marketscape Insights focuses on post-acute facilities, Trella Health has generated readmission metrics specifically for home health agencies, skilled nursing facilities, and hospices.
![]() For more information, see Inpatient versus post-acute readmission rates, below.
For more information, see Inpatient versus post-acute readmission rates, below.
% Hospitalization
In the most general terms, a hospitalization event is when a patient is admitted to a hospital during a post-acute stay or within 30 days after discharge from post-acute care. A hospitalization rate is the percentage of patients treated by the post-acute facility who were admitted to inpatient care. The difference between a readmission rate and a hospitalization rate is that a hospitalization rate does not require a prior inpatient stay and discharge, nor does the hospitalization need to take place within 30 days of inpatient discharge.
% Hospitalization - 30, 60, 90
Since % hospitalization doesn't require a previous inpatient stay and it is not limited to a 30 day period, Trella Health has calculated metrics for patients hospitalized within 30, 60, or 90 days of the start of care date for the type of post-acute care being considered.
![]() For more on Hospitalization, see:
For more on Hospitalization, see:
Readmission 30, 60, 90
A readmission is a 30 day set of events - inpatient discharge to inpatient readmission; all within 30 days. Trella Health has also calculated 60 day and 90 day readmission rates that follow the same requirements: a patient is discharged from inpatient care, and within the time period, the patient is re-admitted to inpatient care. The additional 30 and 60 day rates are calculated the same way, and may have instances of post-acute care within the time frame.
Broken out by Diagnosis or Trella Health Diagnostic Groups
Many tables on Analyze pages include patients treated by a specific facility with related readmission rates broken out by MS-DRGs, Trella Health Diagnostic groups or other clinical breakdowns. These distinctions will show if a specific provider has higher or lower readmission rates for specific populations of patients.
Usage
![]() Readmission rates are one of the most critical metrics for evaluating all facilities involved with a patient's care path. The ideal is for this rate to be low. Compare readmission rates between similar types of providers and against national or regional benchmarks. As always, you will want to compare your agency's readmission rates with your competitor's.
Readmission rates are one of the most critical metrics for evaluating all facilities involved with a patient's care path. The ideal is for this rate to be low. Compare readmission rates between similar types of providers and against national or regional benchmarks. As always, you will want to compare your agency's readmission rates with your competitor's.
Calculation
Overview
All readmission metrics are calculated from multiple claim events. These combined events are considered a readmission when a patient is discharged from an inpatient stay and is readmitted to inpatient care again within 30 days. This readmission scenario could include a post-acute stay, or multiple post-acute stays during that 30 day period.
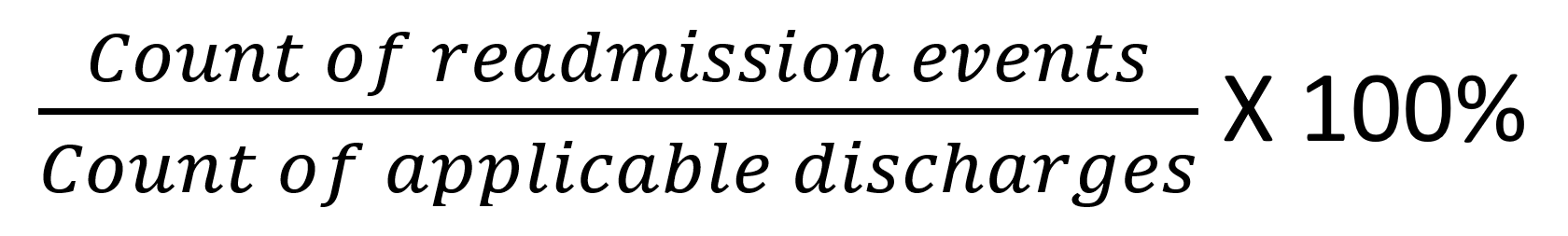
![]() The following basic equation shows how this rate is calculated.
The following basic equation shows how this rate is calculated.
![]() A bunch of clarifications!
A bunch of clarifications!
- "Applicable discharges" in this equation could be a variety of patient populations depending on the facility, agency, or focus of the specific metric. For example, the complete population could be:
- A group of post-acute admission events. (that is, to hospice or home health.) We would not count a discharge that does not include a post-acute admission for a readmission rate for a post-acute agency.
- Count of inpatient discharges - note that this is different from count of distinct discharged patients
- The numerator in this equation is limited to facilities identified under the taxonomies: General Acute, Rural, of Critical Access hospitals.
- Planned admissions are not counted as a readmission, and will not be counted in the numerator.
- Numerator - For any single discharge we we only count a single readmission event. This way, if a patient is in and out of inpatient care multiple times within 30 days, each "pair" of events only counts as one readmission.
- Denominator - when generating our "applicable discharges," we exclude patient discharges with a status code of "02" - transfer to another hospital.
- Inpatient Rehab Facilities stays are not counted in readmission metrics.
Reporting Periods
There are a number of different reporting periods that we use to generate our metrics. To calculate readmission rates we use offset two-year and offset one-year reporting periods. The reason we offset the reporting period is to allow a 30 day reference period for a readmission to take place after the initial inpatient discharge (see images below.)
![]() Our Process: To identify the matching claims that generate our readmission rates, we first look in a specified reporting period and identify inpatient discharges. Each inpatient discharge is an "index event." We then search through the following 30 day reference period to identify corresponding inpatient admissions. Once we find the pair of events, we have identified a readmission.
Our Process: To identify the matching claims that generate our readmission rates, we first look in a specified reporting period and identify inpatient discharges. Each inpatient discharge is an "index event." We then search through the following 30 day reference period to identify corresponding inpatient admissions. Once we find the pair of events, we have identified a readmission.
Reporting Period for most Readmission Rates

Most Readmission Rates in Marketscape use an offset two year reporting period. We identify inpatient discharges during this two-year (24 month) period. The end of this two-year period is offset from the end of the most recent data set by 30 days. In order to get a full 24 months of re-admissions, we use a 25 month reference period within which we identify the inpatient REadmission.

Trended Readmission Rates

The Trended Readmission Rates (found on the Analyze pages in the Utilization and Quality tab) are calculated using an offset one year reporting period. The end of this one-year period is offset from the end of the most recent data set by 30 days. In order to get a full 12 months of re-admissions, we use a 13 month reference period within which we identify the inpatient REadmission.

![]() Because the trended readmission rates are calculated using a one year period, this metric will not match other readmission rates listed under the last reported quarter in other locations in Marketscape for the same organization. In addition, because of the shortened reporting period, you will notice a higher number of readmission rates that are not reported to comply with privacy suppression.
Because the trended readmission rates are calculated using a one year period, this metric will not match other readmission rates listed under the last reported quarter in other locations in Marketscape for the same organization. In addition, because of the shortened reporting period, you will notice a higher number of readmission rates that are not reported to comply with privacy suppression.
Inpatient versus post-acute readmission rates
Our discussion up to this point has been largely focused on readmission rates for inpatient hospitals.
We also calculate readmission rates for post-acute agencies. Here is how:
- Remember that we look for every readmission event; a combination of a INP D/C and a INP Admission within 30 days.
- We then compile every post-acute admission that happens between the two.
- As you can see from the image below, we have what we need for a post-acute readmission metric.

![]() The following equation shows the calculation:
The following equation shows the calculation:

![]() For this equation, PAC Admission would always be for the same post-acute facility.
For this equation, PAC Admission would always be for the same post-acute facility.
Another way to visualize this is:
Numerator: INP D/C ![]() PAC Adm
PAC Adm ![]() INP Adm within 30 days
INP Adm within 30 days
Denominator: INP D/C ![]() PAC Adm within 30 days
PAC Adm within 30 days
Deep in the weeds: Exceptions/Inclusions
![]() For a "set" of claims relative to a specific patient to be counted in an inpatient readmission rate, there does not need to be a post-acute admission between discharge and re-admission. Additionally, the "set" of claims could have multiple post-acute admissions in between and still apply.
For a "set" of claims relative to a specific patient to be counted in an inpatient readmission rate, there does not need to be a post-acute admission between discharge and re-admission. Additionally, the "set" of claims could have multiple post-acute admissions in between and still apply.
Examples of readmissions: (all claim events happen within 30 days of the first INP D/C)
INP D/C ![]() INP Admission (Adm)
INP Admission (Adm)
INP D/C ![]() PAC Adm
PAC Adm ![]() INP Adm
INP Adm
INP D/C ![]() HHA Adm
HHA Adm ![]() HOS Adm
HOS Adm ![]() INP Adm
INP Adm
Which PAC gets the "Credit" for a readmission?
The examples above are relative to understanding readmission rates for hospitals, that is, inpatient care. The metrics would be readmission rates for listed hospitals. When we calculate readmission rates for post-acute agencies, the claim for post-acute admission will occur in the sandwich between the inpatient discharge and readmission, as this image shows:
INP D/C ![]() PAC Adm
PAC Adm ![]() INP Adm
INP Adm
In this case, the readmission rate for the post-acute care agency is limited to patients admitted to post-acute care at the specific agency.
The following scenario is a bit more complicated. Imagine that a patient is admitted to two post-acute agencies between the inpatient discharge and readmission.
INP D/C ![]() PAC1 Adm
PAC1 Adm ![]() PAC2 Adm
PAC2 Adm ![]() INP Adm
INP Adm
In this case, only the second post-acute agency gets a readmission count towards the final readmission rate. The reason we do this is to indicate a higher level of responsibility to the agency that provided the most recent care prior to the readmission.
Unique SNF metrics
If you are digging around in our SNF Product, you will notice that we have a 60 day and 90 readmission rate. In short, we calculate these two metrics in the same way as the 30 day readmission rates, but use 60 and 90 day reference periods for identifying the corresponding inpatient REadmissions. The reporting periods for these metrics are also offset further from the end of the data set to provide the the 60 or 90 day reference period required.