Overview
The Hospitalization Rate is a critical metric that shows up in numerous places in Strategy. In the most general terms, hospitalization means a patient went to a hospital while receiving or within 30 days after discharge from post-acute care. The hospitalization rate is the percentage of patients treated who are admitted to a hospital during their stay or within 30 days of discharge from post-acute care.
![]() The exact meaning of a specific hospitalization metric, and how it is calculated, could be different depending on the provider to which it applies, OR the location in Strategy. In addition, the same metric has different names in different places, or the same name for different metrics. Possible names:
The exact meaning of a specific hospitalization metric, and how it is calculated, could be different depending on the provider to which it applies, OR the location in Strategy. In addition, the same metric has different names in different places, or the same name for different metrics. Possible names:
- Hospitalization Rate
- % Hospitalization: +30 days
![]() Physicians and hospitals do not have hospitalization metrics.
Physicians and hospitals do not have hospitalization metrics.
Similar Metrics
Readmission rates are a similar metric, and understanding the difference is critical. A readmission is a care event where a patient is admitted to any inpatient stay within 30 days of being discharged from an inpatient stay. A post-acute stay does not need to occur between the initial discharge and the re-admission. When a post-acute stay does occur between the discharge and the readmission, we calculate a readmission rate for the hospital, and for the post-acute agency.
To be counted as a hospitalization, there does not need to be an initial inpatient discharge. This also means that there is no 30 day period during which we would count a re-admit. The post-acute stay against which a hospitalization is counted can be a single day or any length of time, and we include if a patient is admitted to a hospital during the 30 days after discharge from the post-acute stay.
![]() Because Readmission rates will almost always be a subset of Hospitalization rates, hospitalization rates will always be higher for any post-acute agency.
Because Readmission rates will almost always be a subset of Hospitalization rates, hospitalization rates will always be higher for any post-acute agency.
![]() For more information on Readmission rates, click here.
For more information on Readmission rates, click here.
Usage
![]() Hospitalization is a performance metric that identifies how well a post-acute agency is succeeding in keeping patients out of the hospital. As a key metric for differentiation, comparing your hospitalization rates with your competitors will provide some insights, but will also require further evaluation.
Hospitalization is a performance metric that identifies how well a post-acute agency is succeeding in keeping patients out of the hospital. As a key metric for differentiation, comparing your hospitalization rates with your competitors will provide some insights, but will also require further evaluation.
- If your hospitalization rates are lower than your competitor(s) this shows that, in general, your agency is providing better patient care. You can use this metric as a talking point for a physician or hospital to refer patients.
- In contrast, if your hospitalization rates are higher than your competitor(s) this presents a challenge. You will need to evaluate your processes and care given to improve your performance.
-
But Wait!! Before you are elated or dismayed, there are other factors at work here. You will need to compare some other metrics.
- Patient Acuity - An agency that is treating more acutely ill patients will have a higher likelihood of having higher hospitalization rates - those patients require more significant care. Check out the Patient Diagnostic Mix table to compare the diagnoses in your patient mix.
- Patient count and hospitalization history - With a smaller patient count, a population of more acute patients will move the metric far more than when "hidden" in a larger population of patients. You need to compare apples to apples.
Calculation
![]() The Trella Health hospitalization rate is the percentage of all admissions to the listed post-acute agency that were admitted to a hospital during their stay or within 30 days of discharge.
The Trella Health hospitalization rate is the percentage of all admissions to the listed post-acute agency that were admitted to a hospital during their stay or within 30 days of discharge.

A few notes:
- Notice that the calculation says "admissions" in the numerator and denominator. If a specific patient is admitted to post-acute care and then admitted to a hospital multiple times during the reporting period, that pair of events will be counted each time.
- The reporting period for this metric is for two years; aligning with the end of the most recent dataset included in Marketscape.
- The index event, the home health admission, must fall in that two year period.
Where can I find this metric?
Strategize page
On the Strategize page, each table has an instance of hospitalization, as shown. In the Path Detail table, we have included the state hospitalization benchmark for comparison.

Analyze page
There are numerous locations with tons of detail for this metric. The images below show what you are looking for and the chart at the bottom will show which providers have these metrics.
Insights
The hospitalization rate can be found in the Insights section for home health and hospice agencies.

Hospitalization Rate - Quarterly Trended
In the Quality tab for SNFs and home health and Quality and Operational tab for hospice, the following table includes a trended hospitalization for the most recent four quarters in our dataset.
![]() At a glance, you can see whether the selected agency's hospitalization rate is trending up or down over the most recent quarters.
At a glance, you can see whether the selected agency's hospitalization rate is trending up or down over the most recent quarters.

![]() For these trended metrics, we use a one year reporting period from which we look for post-acute admissions with a matching hospital admission during the stay or within 30 days of discharge. This is in contrast to the two year reporting period for all other hospitalization metrics in other tables.
For these trended metrics, we use a one year reporting period from which we look for post-acute admissions with a matching hospital admission during the stay or within 30 days of discharge. This is in contrast to the two year reporting period for all other hospitalization metrics in other tables.
![]() Because these trended rates are calculated from a different reporting period, they will not match other hospitalization rates. Remember that we calculate similar metrics in different ways in order to provide different insights. These trended rates tell a different story about the provider.
Because these trended rates are calculated from a different reporting period, they will not match other hospitalization rates. Remember that we calculate similar metrics in different ways in order to provide different insights. These trended rates tell a different story about the provider.
![]() Please don't look for how this is a "12-Month Rolling" metric. Obviously this is a quarterly metric... no matter how it rolls.
Please don't look for how this is a "12-Month Rolling" metric. Obviously this is a quarterly metric... no matter how it rolls.
Hospitalization Rates within 30 and 90 Days from Start of Care by Acuity
These tables contain a breakdown of patient diagnoses for the selected facility categorized by acuity. We calculate the hospitalization rate for each acuity level and diagnoses. In addition, we provide a county and state benchmark for each for comparison.
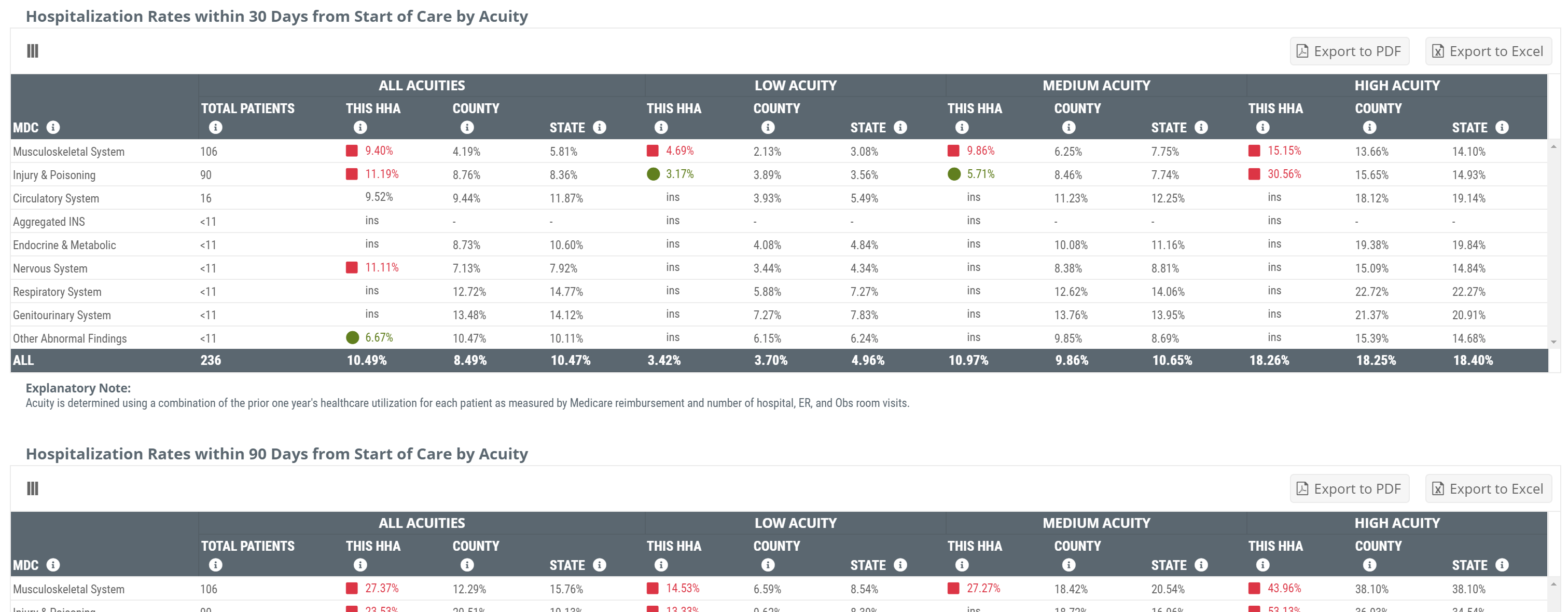
![]() There are two major differences between the metrics in these tables and our "general" hospitalization metric.
There are two major differences between the metrics in these tables and our "general" hospitalization metric.
- The reporting period for these tables is a bit unusual. The patient counts, like most counts, are calculated from a one year period. The hospitalization rates, however include admissions from the same two year period as other hospitalization rates. We use different period so that multiplying a count by a percent can't generate a count <11.
- The reference period for hospitalization is not any time during the patients stay or within 30 days of discharge. These metrics capture a very specific time period after post-acute admission; 30 days or 90 days. That is, we only count patients with high-acuity circulatory system diagnoses who were admitted to post-acute care and then hospitalized within 30 days of admission.
![]() For more information about these tables, click here.
For more information about these tables, click here.
Hospice only - Length of Stay by Diagnostic Category - % Hospitalized: +30 Days
The hospitalization metrics in this table have the same parameters as the general hospitalization metric; a two-year reporting period, and hospitalizations during the stay or within 30 days of discharge. The difference with these metrics is that the rate in each row is calculated only for patients with the diagnostic type in the row. County and state benchmarks for the same diagnosis are provided for comparison.
For example, using the image below, the hospitalization rate for the selected hospice of 2.1% in the top row is for all patients with circulatory system diagnoses who were admitted to the hospice during the two year reporting period who were admitted to a hospital during their stay or within 30 days of discharge.

![]() Although the Diagnostic Category header includes, (MDC), there is no connection to CMS's Major Diagnostic Categories. The diagnostic categories in this table align with the Trella Health Diagnostic groupings.
Although the Diagnostic Category header includes, (MDC), there is no connection to CMS's Major Diagnostic Categories. The diagnostic categories in this table align with the Trella Health Diagnostic groupings.
For more information on Trella Health diagnostic groupings, click here.
Location Summary
| Location or Table / Provider Type | Skilled Nursing | Home Health | Hospice |
| Insights (Hospitalization Rate) | |||
| Hospitalization Rate - (12 month rolling) |
(Under Quality tab) |
(Under Quality tab) |
(Under Quality and Operational tab) |
| Hospitalization Rates within 30 Days from Start of Care by Acuity |
(Under Quality tab) |
(Under Quality tab) |
|
| Hospitalization Rates within 90 Days from Start of Care by Acuity |
(Under Quality tab) |
(Under Quality tab) |
|
| % Hospitalized: +30 days - In Length of Stay by Diagnostic Category table |
|
(Under Quality and Operational tab - includes county and state benchmarks) |