Overview
The Home page is where you get a broad overview of a network you have created, or a network that was shared with you. Once you have selected a network, the page will show some of the most critical metrics. You will also be able to drill down on specific metrics by clicking the "Details" button. This article covers three aspects of this page:
- Page Basics - an overview of the features and metrics on the Home page
- Understanding the Metrics - A summary of the metric on each tile
- PMPM Details - When you click on the "Details" button on the PMPM tile, new content is available. This section includes the definitions for the metrics in the tier two tables
![]() If you navigate away from the Home page and return, the same network you selected will be visible.
If you navigate away from the Home page and return, the same network you selected will be visible.
Page Basics
The Strategy Home page is where you can view a summary of metrics for a chosen network.
![]() The network can be either one that you created or one that was shared with you by another user in your company.
The network can be either one that you created or one that was shared with you by another user in your company.
Please refer to this image for the numbered details below. 
![]() Left Navigation - these buttons allow you to navigate between the pages in Strategy.
Left Navigation - these buttons allow you to navigate between the pages in Strategy.
![]() Metric Definitions - Click this link to open a dialog box that explains the metrics on this page in more detail.
Metric Definitions - Click this link to open a dialog box that explains the metrics on this page in more detail.
![]() Network Selection - Click on this selector to choose the network for which you want to show details on the page.
Network Selection - Click on this selector to choose the network for which you want to show details on the page.
![]() Year Selection - Choose which dataset of metrics you want to display for your chosen network.
Year Selection - Choose which dataset of metrics you want to display for your chosen network.

![]() Network performance metrics - The tiles on this page represent the most important metrics you need to evaluate the chosen network. For a summary of these tiles, see Understanding the Metrics (below).
Network performance metrics - The tiles on this page represent the most important metrics you need to evaluate the chosen network. For a summary of these tiles, see Understanding the Metrics (below).
![]() Risk Adjustment Toggle - To add risk adjustment to the metrics on the page, switch the toggle from off
Risk Adjustment Toggle - To add risk adjustment to the metrics on the page, switch the toggle from off ![]() to on
to on ![]() .
.
For more on risk adjustment, see HCC and Risk Score.
Detail button - 
Some tiles include a "Details" button. What happens when you click on a "Details" button is different depending on the tile.
- PMPM/PMPY tile - Clicking the "Details" button opens a new chart and two new tables on the Home page, see PMPM Details (below)
- Patient Risk Score (HCC) tile - The "Details" button will open the Explore page with the System View "HCC Risk Score."
- All Causes Readmissions tile - Clicking this "Details" button will open the Explore page with the "All Cause Readmissions" System View applied.
![]() You will probably want to keep the Home page open since evaluation of the selected network is what you are working on. Although the PMPM tile is an expansion of the Home page, the "Details" buttons on the other metrics will navigate you away from the Home page. The suggested workflow is to open a new tab in your browser and duplicate the Home page in this new tab before you click the "Details" button.
You will probably want to keep the Home page open since evaluation of the selected network is what you are working on. Although the PMPM tile is an expansion of the Home page, the "Details" buttons on the other metrics will navigate you away from the Home page. The suggested workflow is to open a new tab in your browser and duplicate the Home page in this new tab before you click the "Details" button.
![]() For more information, see Using Views.
For more information, see Using Views.
Understanding the Metrics
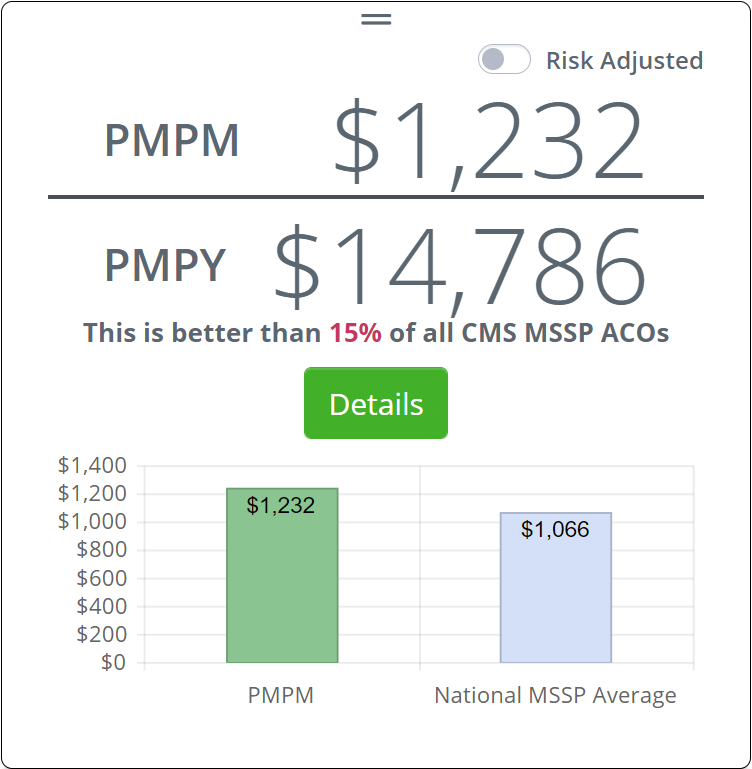
PMPM/PMPY
The Per Member Per Month metric is an important metric for evaluating the performance of the network you have designed. In short, the PMPM metrics is an average of costs per beneficiary attributed to your network calculated for one month. PMPY is the yearly average or, it is the PMPM times 12.
![]() For more information on PMPM, see How do we Calculate PMPM?
For more information on PMPM, see How do we Calculate PMPM?
 Details
Details
 This is better...
This is better...
![]() At first glance, this tile is a bit confusing. The sentence states that "This is better than 15% of all CMS MSSP ACOs," and then the chart shows that your network is more expensive.
At first glance, this tile is a bit confusing. The sentence states that "This is better than 15% of all CMS MSSP ACOs," and then the chart shows that your network is more expensive.
How can more expensive be better?
Remember that you are comparing your network to all CMS MSSP ACOs. Even though your network's costs are higher than the average, your PMPM is still better than some ACOs; in this case, your network is better than 15% of all networks.
The conclusion we draw from this is that we want to drive costs down in our network so that we will get closer to or beat the national average. This will make the percentage of ACOs against which we are "better" increase.
Another way of looking at this is, the goal is to be better than 75% or more of all ACOs out there. To do that, our network needs to get costs down. (Which might mean adding/removing providers from the mix.)
Details
Clicking on the "Details" button opens a new chart and two new tables on the Home page, see PMPM Details (below)
Risk Adjusted toggle - 
We expect that providers that care for more challenging patients will incur more costs to provide patient care. When you turn on the "Risk Adjusted" toggle, the costs in the PMPM tile are recalculated to reflect the risk factor for the network using the risk score of the selected network.
![]() For more information on risk adjustment, just keep reading.
For more information on risk adjustment, just keep reading.
Patient Risk Score
Risk Scores are calculated in accordance with specific and detailed parameters defined by CMS, which include factors such as patient diagnoses and demographics. The Risk Score number can be used to evaluate a specific provider or to compare different providers. In general, a higher number is indicative of a provider that treats patients with greater acuity, that is, patients needing more extensive care.
![]() Although you can use Risk Scores to evaluate and compare providers, the primary use of the Risk Score is to adjust patient costs to make comparison between providers equitable. You expect a provider that treats more acute patients to incur greater costs - Risk Scores allow us to adjust costs so comparisons are more "fair."
Although you can use Risk Scores to evaluate and compare providers, the primary use of the Risk Score is to adjust patient costs to make comparison between providers equitable. You expect a provider that treats more acute patients to incur greater costs - Risk Scores allow us to adjust costs so comparisons are more "fair."
![]() For the complete article, see Risk Scores and HCC.
For the complete article, see Risk Scores and HCC.
![]() Clicking the "Details" button will open the Explore page for the chosen network with the System View "HCC Risk Score" applied.
Clicking the "Details" button will open the Explore page for the chosen network with the System View "HCC Risk Score" applied.
All Causes Readmissions
In short, this is the readmission rate calculated for all applicable providers in the chosen network. A readmission rate is the percentage of discharges re-admitted back into any inpatient care within 30 days of the initial inpatient discharge.
![]() The following basic equation shows how this rate is calculated.
The following basic equation shows how this rate is calculated.
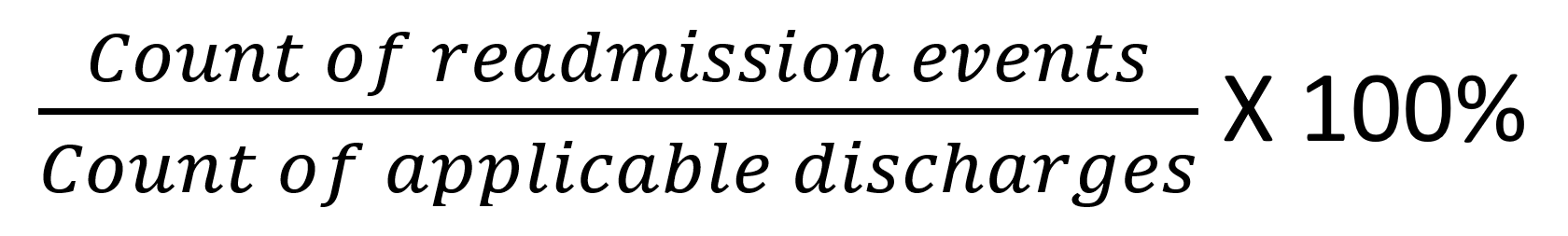
where a readmission event is an admission to inpatient care within 30 days of inpatient discharge.
 This is better...
This is better...
As always, one of the primary purposes of Strategy is to evaluate the strength of your network. In this case, for our chosen network, the readmission rate of 14.70% is better than 61% of all CMS MSSP ACOs.
![]() Clicking this "Details" button will open the Explore page with the "All Cause Readmissions" System View applied.
Clicking this "Details" button will open the Explore page with the "All Cause Readmissions" System View applied.
![]() For a flood of details about this metric, see Readmission Rates.
For a flood of details about this metric, see Readmission Rates.
And the following list contains even more details about this metric.
- This metric represents estimated DCE assigned beneficiaries with an Inpatient admission within 30 days of a discharge from a previous inpatient admission.
- Readmission could be to the same or different Inpatient facility.
- Readmissions into Inpatient Rehabilitation Facilities (IRFs) are not included.
- Planned/elective readmissions are not included.
- Physicians with <11 beneficiaries are excluded from the denominator.
- Lookback period is Dec 1st two years ago through Dec 01 one year ago, depending on the time period selected.
- Percentile represents comparison of the All Causes Readmissions to the All Causes Readmissions of all other MSSP ACOs.
- MSSP ACOs with null or insufficient beneficiaries to calculate All Causes Readmissions are excluded in the comparison.
Patient Population Beneficiaries
This is the count of estimated DCE assigned beneficiaries for the selected Network and Performance Year.
![]() For more information, see How does Trella Health identify Attribution?
For more information, see How does Trella Health identify Attribution?
PMPM 
Some Basics
The tier 2 mode of the home page has a few new features:
![]() Back to Tier 1 - Clicking the left arrow will navigate to tier one for the home page.
Back to Tier 1 - Clicking the left arrow will navigate to tier one for the home page.
![]() Network Selection - You can select which of your networks is displayed on the page
Network Selection - You can select which of your networks is displayed on the page
![]() Risk-Adjusted toggle - On the tier2 page, this toggle adjusts costs for the whole page, not just the PMPM tile.
Risk-Adjusted toggle - On the tier2 page, this toggle adjusts costs for the whole page, not just the PMPM tile.
![]() Performance Year Selection - As you can see from the image above, the selector allows you to make changes to the dataset used to populate the table.
Performance Year Selection - As you can see from the image above, the selector allows you to make changes to the dataset used to populate the table.
![]() County Averages Selection - Using this filter, you can choose one or more counties and the tables below will be limited to providers in those counties.
County Averages Selection - Using this filter, you can choose one or more counties and the tables below will be limited to providers in those counties.
Trended PMPM Chart
The chart to the right of the PMPM tile shows the PMPM monthly trend for the selected year.
To the right of the chart is the YTD Total Spend for the selected network.
![]() Although this chart looks like the network totally tanked in the final quarter, the chart shows zeros for the last three months because the data for the last quarter of 2021 is not available.
Although this chart looks like the network totally tanked in the final quarter, the chart shows zeros for the last three months because the data for the last quarter of 2021 is not available.
Two Tables
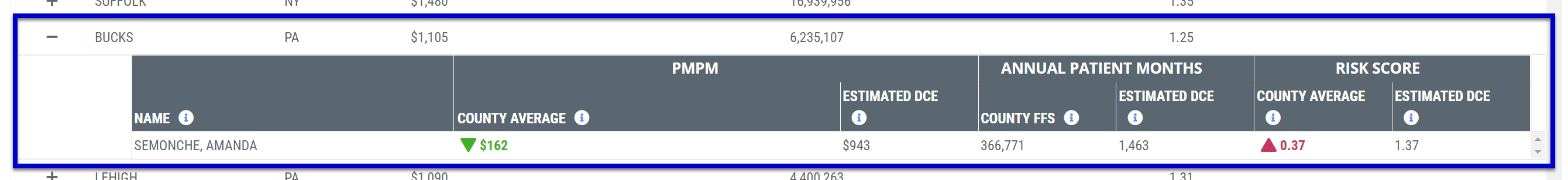
Both tables provide details about physicians. However, each of these tables slices the PMPM metrics from a different perspective.
- The County Averages table is organized by county and you can drill down to the physicians. Of course, you can use this table to glean county level market data. Drilling down to the physician is a wonderful option.
- The Network Physicians table contains all physicians in the network without the regional breakdown.
Opening the tables
When you first navigate to the second tier of the Home page, you won't see the tables. Instead, the tables are rolled up. Click on the > to expand the table.
County Averages
The top table focuses on costs by county. ALL counties for all states included in the network where attributed beneficiaries reside will be included in the table by default.
![]() Use the "County Averages" filter at the top of the page to limit the entries included in this table. You can choose multiple counties at a time.
Use the "County Averages" filter at the top of the page to limit the entries included in this table. You can choose multiple counties at a time.
| Metric/Column | Description |
| County | The name of the county for the row of metrics |
| State | That state for the listed county |
| PMPM - County Average | This is the average per beneficiary, per month spend for all FFS Professional claims with the listed beneficiary county of residence filed during the selected claims year. |
| Annual Patient months - County FFS | This is the total Annual Patient Months (excluding months following beneficiary death) for the Medicare FFS beneficiary population with the listed beneficiary county of residence during the selected claims year |
| Risk Score - County Average | This is the average HCC Risk Score for all Medicare FFS professional claims with the specified beneficiary county of residence filed during the selected claims year |
Physician Details
When you click on the + to the left of the county name, a sub-table opens with metrics for all network physicians who submitted FFS claims for patients residing in listed county.
|
Metric/Column |
Description | |
| Name | The Physician's name | |
| PMPM | County Average | This is the average per beneficiary, per month spend for all Medicare FFS professional claims with the listed beneficiary county of residence filed during the selected claims year |
| Estimated DCE | Average per member, per month spend for the physician's estimated DCE population residing within the listed beneficiary county during the selected performance period | |
| Annual Patient Months | County FFS | The count of Annual Patient Months (excluding months following beneficiary death) for the Medicare FFS beneficiary population with the listed beneficiary county of residence during the selected claims year |
| Estimated DCE | This is the count of DCE Eligible Patient Months for the physician(s) DCE estimated population residing within the listed beneficiary county during the selected performance period | |
| Risk Score | County Average | This metric is the average HCC Risk Score for all Medicare FFS professional claims with the specified beneficiary county of residence filed during the selected claims year |
| Estimated DCE | This metric is the average HCC Risk Score of the physician(s) estimated DCE population residing within the listed beneficiary county during the selected performance period | |
 Patient Months
Patient Months
It has been said that everyone already understands what a "patient month, or a "member month" is. If you are in that group, congratulations, you can move on.
For the rest of us, a little math might help, especially when we see this in the table:
Over 12 million "Patient Months" just seems huge! But what does it represent?
![]() To make the point that we aren't really counting months or patients, let's call this metric "patient-months." (Many in the industry call this "member-months.")
To make the point that we aren't really counting months or patients, let's call this metric "patient-months." (Many in the industry call this "member-months.")
![]() A "patient-month" metric is calculated by adding the number of months of benefits received for each applicable patient (beneficiary) in a specific patient population.
A "patient-month" metric is calculated by adding the number of months of benefits received for each applicable patient (beneficiary) in a specific patient population.
Let's start with one patient. If one patient receives benefits for 12 months, that is 12 patient-months.
But not all patients will receive benefits for 12 months. Some will start as a beneficiary after the start of the reporting period, and others will go off of service before the end of the reporting period.
| Patient | Months of Service |
| Mary Doe | 12 |
| Jeff Doe | 8 |
| Fred Doe | 6 |
| Billie Doe | 12 |
| Total patient months | 38 |
In short, we add together the months of service for all patients in the chosen population.
Patient Population - In the case of the County Averages table, the patient we use for the total patient-months count are all patients in the listed county who are members of the selected network. The count of patient-month could be all patients in a specific network, or members of a specific insurance provider
Network Physicians
This table shows all physicians in the selected network.
| Metric/Column | Description | |
| Name/NPI | Physician's name and NPI | |
| State/City/County/ZIP | The primary state, city, county, and ZIP code where the listed physician practices. | |
| Specialty | This is the physician's self reported primary specialty as listed in the NPI file. | |
| PMPM | Estimated DCE |
This metric is the total per member, per month spend for the physician DCE estimated population in the performance year (PMPM)
|
| All | This is the total per member, per month spend for all patients for whom the physician is listed as the attending or performing physician on a FFS claim in the performance year (PMPM) | |
| Beneficiary Patient Count | Estimated DCE | DCE estimated population for the performance year |
| All | This metric is the count of patients for whom the physician is listed as the attending or performing physician on a FFS claim in the performance year | |
| Risk Score | Estimated DCE | Average HCC Risk Score of the physician DCE estimated population |
| All | Average HCC Risk Score of patients for whom the physician is listed as the attending or performing physician on a FFS claim in the performance year | |